Eloise's {Almost} Home Birth Story (Part 1/3)
/We're back with another Delmarva Community Birth Story. This time, it's from a special THRIVE client who planned and *almost* had a home birth. When she originally shared this on her own blog, I HAD to ask her to share it here, too. It's just so beautifully written and such a fantastic story of all things that encompass birth and motherhood: Joy, love, frustration, trust, patience, strength, and humility. Enjoy! xo--Maria
We'd been married for just barely a year. We weren't *trying* to get pregnant, but...I would not have minded. It was a Friday morning, July 15th 2016. The next day Jake and I would be leaving to spend just under a month in the mountains of Virginia for his Young Life summer assignment. My cycle was due to start the coming Tuesday, and I decided to take a test before we left town.
Our world was changed forever.
I always knew that I wanted to have a natural birth. My mother delivered me and all four of my siblings without pain medication and I always admired her determination. I devoured books and articles and all kinds of literature on the subject of natural birth and grew in my conviction that medication-free delivery was what was best for me and my baby. I have fibromyalgia and I was nervous about the amount of pain and fatigue my body would be able to endure, so I began looking for ways to prepare myself and my body to give birth naturally - breathing, relaxation, visualization. I also began searching for a doula to support me during delivery. The hospital I planned to give birth in has a 95% epidural rate and an alarming 30% c-section rate. My CNM advised me that if I wanted a natural birth, a doula was a MUST. I made some inquiries and was connected with a wonderful doula service, and met with Chloe for a consultation. I told her all about my determination to have a natural birth but my fears surrounding giving birth in the hospital and my physical challenges with fibromyalgia. She was so affirming and validating towards my desires that I began to cry with relief in the middle of our meeting.
"Have you ever considered having a home birth?"
No. Not me. Or at least, it sounds wonderful, but this is my first baby. My husband would never agree to it. We need the security of the hospital for our first go-round. I'm already over 30 weeks along, it's too late to consider something like that.
"Maybe just think about it."
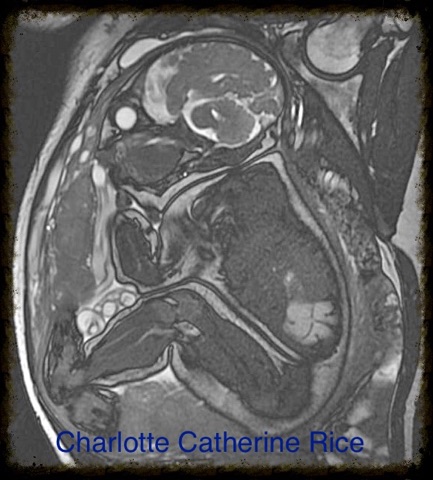
Obviously, we hired Chloe. She never said another word about home birth but the idea was lodged in my brain and heart. Again, I hit the books. I learned that the US has the worst infant mortality and maternal death rates among every developed country, even though we spend the most money on maternity care. I learned that our C-Section rate is double what the World Health Organization recommends, and that many of these are completely preventable if routine interventions could be avoided. I learned that the developed countries who most utilize home birth midwives have the best results. I learned that home birth recently became legal in my state, and that home births have been shown to be associated with fewer maternal interventions and deaths. I asked Chloe to help me find more information about how to have a home birth in Delaware, and was surprised and excited to learn that she was actually a student midwife in addition to being a doula, and was working alongside a Certified Professional Midwife named Susan who lived not even an hour from my home! I knew in my heart that this was what I wanted, but was still convinced that it was too late in the game to make such a big decision, that we could never afford the fee, that there was no way.
Jake and I met with Susan and Chloe and discussed what it would look like for us to have a home birth with them. We both had a lot of questions: How would prenatal visits look since I'm so far along? What would cause you to make the decision to transfer to the hospital? What signs would you be watching for and at what point in the process would you make that call? What kind of emergency medication and equipment do you carry? What would happen in case of any unforeseen circumstances? I realize now after going through all of these things how difficult my questions must have been to answer, because every case is so different. But they were patient and reassuring and even Jake, who previously had NO peace surrounding the idea, became convinced that this was the best call for our family! We were going to do it - we were going to have a home birth!
{{{PART 2 COMING TOMORROW!}}}