The Birth That Changed My Life: Part II
/This week in our Delmarva Community Birth Stories series, we're doing something a little different. This story is shared by Thrive owner and doula, Maria Mengel.
If you haven't read Part I yet, hop on over and check it out now.
I received the worst message that you could ever receive as a friend/doula:
"Amniotic fluid is basically zero. They can't find any kidneys or bladder. Without kidneys, the baby will die after birth. We're going to AAMC for induction. You should come now."
Then it was followed by:
"worst nightmare"
I was completely in shock and "respond" mode. I was in the shower, so I jumped out, toweled off, texted my husband to come upstairs now, and started getting ready. I was in the car within minutes. I was nervous, scared, worried about my friends and their baby, and in a real hurry to get there. On my way, I called and talked to my mom and my doula/mentor to keep my mind from racing too much. They both promised to pray and reassured me that I would be able to support my friends no matter what. I told them that it wasn't fair that my first bereavement birth after receiving my certification was for my best friends. I was still feeling pretty raw from the sudden death of my little brother just months before, and I truly didn't know if I could do it.
I didn't waste any time, but I didn't speed either. While I was alone in the car, I tried to think about everything that I learned about babies who passed after birth. I would need to be strong enough to explain to my friends what to expect and yet compassionate enough to support them through a potentially long induction and birth. Two hours later, I pulled into the hospital parking garage. I practically ran to the elevators, through the Labor and Delivery doors and down to the room where the nurse told they would be. I quietly opened the door to my friends sitting on a couch together talking with their midwife.
I was breathing heavily from running and when I walked in it was completely silent.
Without speaking, I walked across the room and sat down with my friends when Wes said "Well, the induction is not until Monday". Apparently Labor and Delivery was really busy that day (Friday), so they decided to wait until Monday for the induction. Their baby had been surviving with extremely low amniotic fluid levels and seemed to be doing fine for some time (they estimated up to 6 weeks or so), so they figured a few more days probably wouldn't make a difference. Everyone seemed so relieved.
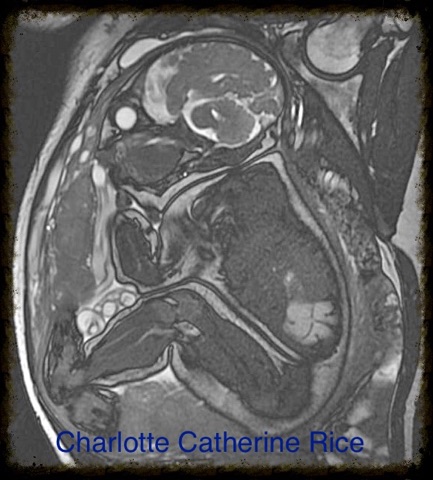
It was kind of awkward because we were all in shock, sad, relieved, and scared at the same time. The midwife came back with a specialist on the phone from Children's National Health System in DC. He expressed his apologies about their situation but offered them a pretty innovative opportunity. He told them that he could see them early Monday morning for a fetal MRI to get a closer look at baby's renal system and lungs. He told them that he would hopefully be able to get a more concrete diagnosis before the induction that morning so that they would know how to prepare for their baby's treatment after birth. They decided to accept the offer and scheduled an MRI in Washington D.C. at 7:30am and an induction in Annapolis at 9am.
We spent the next hour or so on the phone making appointments and then made the two hour trip back home to the Eastern shore. Meghan's parents were on their way from upstate New York and they needed to stop at the grocery store to stock their fridge for guests. Wes took my husband to the store with him while Meghan and I stayed at my house with the girls. Meghan and I talked about how it all seemed so strange and so awkward that we just found out that her baby might die and we were doing normal things like grocery shopping and watching my kids play. When they went home that night, I promised to stay in touch.
Guys, thank God for texting.
We spent the time between her diagnosis and her birth texting constantly. It was so much easier for Meghan to express her thoughts and feelings through texts than saying it all out loud. Our relationship as friends grew leaps and bounds through those messages, many of which I saved so that I wouldn't forget. The good and bad feelings, the fears, the worries, the logistics,etc. It was like having a diary to process our thoughts together. And it was so much easier to text our thoughts than say them out loud.
On Sunday, we scheduled our prenatal meeting together. It was supposed to be a meeting where we discussed their dreams and desires for their beautiful water birth. But instead, I got my first taste of what it was like to be a bereavement doula. I met with Meghan and Wes and we discussed their options. If the MRI the next day confirmed their worst fears, and baby truly did not have a bladder or kidneys, and severely underdeveloped lungs, they would have a few choices. The staff at their hospital informed them that they could continue with the induction the next day, with the understanding that the baby might not make it through the stress of labor and die before birth. Or they could wait for spontaneous labor, knowing that the baby may pass before labor begins, and then definitely deliver a stillborn baby. Or, they could schedule a cesarean to guarantee that Meghan and Wes would have a chance to meet and hold their baby still alive, and then know that baby would probably pass in her arms shortly after.
We talked about what to expect with all of the options, including the details that I didn't ever want to have to share with my friends.
They were aware that funeral arrangements would have to be made, but weren't ready to talk about it yet, so Meghan's mother and I talked through their options and I contacted a funeral home, asked questions about their options in terms of transportation of the baby's physical form and services. I gathered all of that information and placed it in a folder in my birth bag. They decided to wait until after the MRI in the morning to make a final decision about their birth plans.
The next morning, I knew that it would likely take a long time before the MRI was finished and they were able to talk with all of the necessary specialists in DC, so I did the only thing I could think of to pass time. I feverishly cleaned my house. I literally was scrubbing the freaking baseboards because if I sat still too long, I started getting sick thinking about what might happen later that day. I had a knot in the pit of my stomach and every once in a while, I had to sit down and mentally tell myself that what they were about to go through was much harder than my role in the process, and that I could support them 100%. I knew that there would be a lot of processing and healing time afterward for everyone and I planned to give myself the energy and space for that after the birth.
When Meghan finally called, she told me that the news wasn't good. They were unable to find any bladder or kidneys still. They told her that her baby's lungs were severely underdeveloped (as a result of the low amniotic fluid) and that her worst nightmares were confirmed. Life outside of the womb for their baby was highly unlikely. They weren't going through with the induction. They were coming home and waiting for their baby to decide when it was time to be born. They were aware that there was a risk of stillbirth, but they wanted to respect their baby's timing.
Baby Rice's diagnosis:
• Bilateral Renal Agenesis
• Pulmonary Hypoplasia
• Anhydramnios
• Potential slight spinal malformation
I was absolutely heartbroken for my friends. And I was so relieved to know that today wasn't the day.
We didn't know it at the time, but we still had another two whole weeks before their baby was born. They decided after the MRI to find out the sex of their baby so that at least for a short while alive, their baby could have a name. Here is the MRI photo of Charlotte Catherine Rice.
**Click here to continue to Part III**
***Of course, I have received full permission from Meghan and Wes to share my version of this story and use their real names***