What Do Amniotic Fluid and Tacos Have in Common?
/She's 9 months pregnant and strolling the aisles of the grocery store picking up last minute things to make freezer meals before her baby comes. Her water breaks and there's a big gush of fluid rushing down her legs onto the floor. Contractions start immediately and she's panting and groaning through them. Everyone rushes to get her in a car and the vehicle flies through traffic lights and stop signs to get her to the hospital just in time for her to scream her baby out. EMERGENCY!!!
I hope you already know that it rarely ever happens that way. And if you didn't know, I'm here to tell you: It probably will not happen like that to you. In fact, only about 10% of women have their water break before labor starts. The majority of waters rupture well into the labor process, and quite often, very near the end.
Now I bet you're wondering why the title has the word "tacos" in it, huh? Well, if you've given birth before, you've probably experienced a situation where your care provider asks you if your water has broken yet. If the answer was yes, they may have asked you a few questions about it. Check those questions out now so you know what to look for next time and can be prepared to answer them! If your water breaks, remember "TACO":
T (Time):
What time did your water break? Care providers will want to know how long your membranes have been ruptured. In most cases, there are protocols for how long you can have ruptured membranes before birth. The concern is an increased risk of infection, as your protective bag of waters is no longer surrounding your little baby inside. If your water broke and you're not already in active labor, remember to limit the risk of infection by not inserting anything into the vagina, including tampons, fingers, having intercourse, etc. Take showers instead of baths. Remember, each time something (even a gloved finger from a care provider) is inserted, the risk of infection goes up.
A (Amount):
Was it a huge gush of fluid that came out like a waterfall? Or did you happen to feel a few small leaks here and there? Could the leaks have been urine? Have you had sex recently? Could the leaks have been semen? Could the leaks or fluid be vaginal discharge? Many women experience a lot of discharge in late pregnancy. Those may sound like silly questions, but they all happen and that's okay!
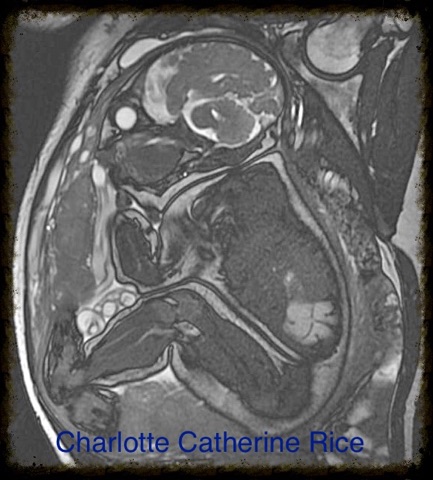
C (Color):
What color was the fluid? Normal amniotic fluid is colorless and sometimes a bit cloudy. Occasionally it is lightly tinged with small amounts of blood or mucus. Sometimes it has white flakes in it, which is just vernix that came off of baby's skin. The reason why they ask this question is because sometimes the fluid can be slightly or heavily tinted with meconium. Sometimes, baby passes his/her first stool while still in utero. This is common and very rarely an indication of a problem, but the care providers like to know because each hospital has a different protocol for how to respond to this situation. In our local hospital, they invite a respiratory therapist into the labor and delivery room just before birth. The respiratory therapist stands in the back and out of the way. If the baby has trouble breathing on his/her own, the therapist is there to help, so the baby doesn't aspirate any of the meconium in the water. Usually the baby is born, cries and breathes just fine, and the therapist quietly slips back out. If you're concerned about this or would like to know the protocol in your own hospital, make sure to ask your care provider during your pregnancy.
O (Odor):
What does it smell like? Yep, you gotta smell it to answer this question. Either your underwear or a sanitary pad that you're wearing. Most people describe amniotic fluid as smelling odorless, sweet, clean, or like semen. I suppose each person thinks of it differently. Here's why we smell it. We want to make sure it doesn't smell like urine, which has a distinctive smell. And we want to make sure it doesn't smell foul. Foul smelling amniotic fluid can be a symptom of a uterine infection that you'll want to get checked out. In most cases, though, you're just trying to determine if it's amniotic fluid or urine.
So, there you have it. Tacos and amniotic fluid DO have something in common! If you think your water has broken or are unsure, go through these little questions yourself so you already know your answers for when you call your care provider.